In today’s world, infertility is no longer a taboo subject, and many couples are seeking various fertility treatments to have a child. One of the most commonly used treatments for infertility is in-vitro fertilization (IVF), which involves fertilizing the egg outside the body in a laboratory dish and then transferring the resulting embryo to the uterus. IVF is a complex process that involves many steps and can be overwhelming for those who are considering it.
While IVF can be a challenging journey for couples who are struggling with infertility, it has given hope to millions of couples around the world. It is essential to have a thorough understanding of the process to make informed decisions and to be mentally prepared for the journey ahead. This guide will provide you with all the information you need to know about the step-by-step process of IVF, making your journey to parenthood a little smoother.
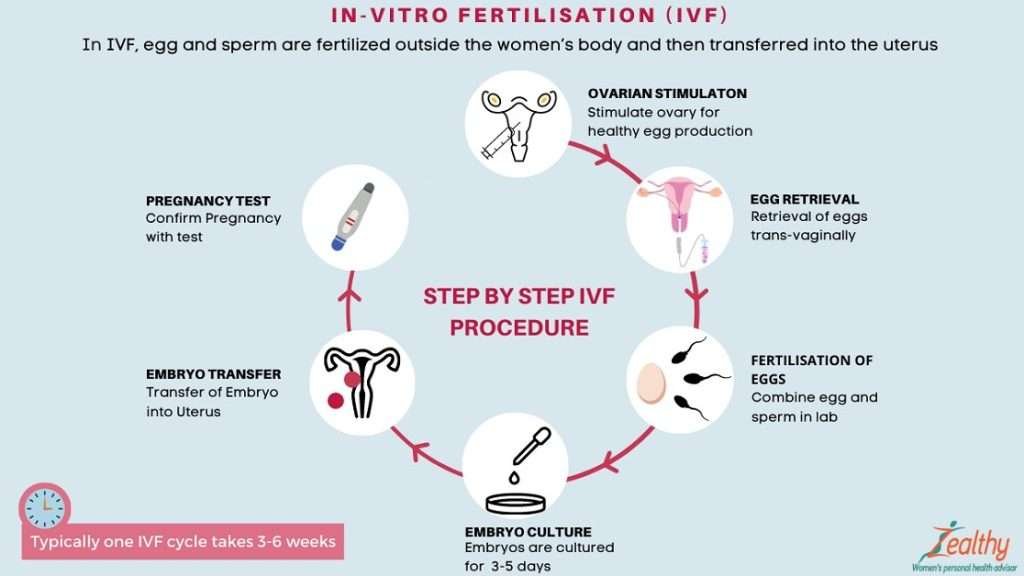
step-by-step process of IVF
In this complete guide, we will walk you through the step-by-step process of IVF. From ovarian stimulation to embryo transfer, we will cover all the essential steps of the IVF process, including the risks and potential side effects. We will also discuss the emotional and financial investment required for IVF and provide tips on how to prepare for each stage of the process.
Step 1: Ovarian Stimulation
The first step in the IVF process is ovarian stimulation. The goal of ovarian stimulation is to encourage the ovaries to produce multiple eggs. Typically, only one egg is released during ovulation, but in IVF, multiple eggs are needed to increase the chances of a successful pregnancy.
To stimulate the ovaries, hormonal medications are prescribed. These medications are usually given in the form of injections and are designed to increase the number of follicles that develop in the ovaries. Follicles are small fluid-filled sacs that contain an immature egg.
During ovarian stimulation, monitoring is critical to ensure that the ovaries are responding appropriately to the medication. This monitoring is typically done through transvaginal ultrasound and blood tests. Ultrasound allows doctors to visualize the follicles and measure their size, while blood tests measure hormone levels.
While ovarian stimulation is a crucial step in the IVF process, it does come with some risks. The most significant risk is ovarian hyperstimulation syndrome (OHSS), which occurs when the ovaries become overstimulated and produce too many follicles. OHSS can cause abdominal pain, bloating, and nausea, and in severe cases, can be life-threatening.
To minimize the risk of OHSS, doctors may adjust the dosage of the hormonal medications or delay the egg retrieval procedure. In rare cases, IVF may need to be canceled altogether if there is a significant risk of OHSS.
Step 2: Egg Retrieval
Once the follicles have reached an appropriate size, the eggs are ready to be retrieved. Egg retrieval is a minor surgical procedure that is done under sedation. During the procedure, a thin needle is inserted into the follicles through the vaginal wall, and the eggs are aspirated.
The egg retrieval procedure takes around 20-30 minutes to complete, and patients are usually discharged from the clinic within a few hours. Some mild cramping and discomfort may be experienced after the procedure, but it typically subsides within a few days.
After the eggs have been retrieved, they are transported to the laboratory for fertilization. The eggs are then placed in a petri dish with sperm, and the fertilization process begins. In some cases, a single sperm is injected into the egg using a technique called intracytoplasmic sperm injection (ICSI).
Once fertilization has occurred, the embryos are monitored for growth and development. The embryos are usually kept in the laboratory for 3-5 days before being transferred to the uterus.
It’s worth noting that not all eggs retrieved will be fertilized, and not all fertilized eggs will develop into embryos. Therefore, it’s essential to have realistic expectations and to understand that success rates vary from person to person.
Step 3: Embryo Culture and Monitoring
After the eggs have been retrieved and fertilized, the embryos are cultured and monitored in the laboratory. The embryos are kept in a special solution and incubated under specific conditions to promote growth and development.
During this stage, the embryos are monitored carefully to ensure that they are developing normally. The embryologist will check the embryos daily for signs of growth, cell division, and quality. The embryos are given a grade based on their quality, with higher grades indicating better quality embryos.
Embryo monitoring is a crucial step in the IVF process, as it allows doctors to select the healthiest embryos for transfer. The number of embryos transferred depends on a variety of factors, including the age of the woman and the quality of the embryos.
In some cases, additional testing may be done on the embryos to check for chromosomal abnormalities. This testing, known as preimplantation genetic screening (PGS), can help identify embryos with a higher chance of success and reduce the risk of miscarriage.
It’s worth noting that not all embryos will develop normally, and some may stop growing or be discarded. It’s also essential to have realistic expectations about the success rates of IVF and to understand that not all embryos will result in a successful pregnancy.
Step 4: Embryo Transfer
Embryo transfer is the final stage of the IVF process. This step involves placing one or more embryos into the woman’s uterus. The embryo transfer is done using a thin catheter, which is inserted through the cervix and into the uterus.
The number of embryos transferred depends on various factors, including the age of the woman and the quality of the embryos. In some cases, only one embryo may be transferred to reduce the risk of multiple pregnancies.
Before the embryo transfer, the woman may be given medications to prepare the lining of the uterus for implantation. These medications help to create an optimal environment for the embryo to attach to the uterine lining.
The embryo transfer procedure is usually quick and painless, and it typically takes around 15-30 minutes to complete. After the transfer, the woman is usually advised to rest for a short time before leaving the clinic.
Following the embryo transfer, the woman will need to wait for around two weeks to find out if the treatment has been successful. During this time, the woman may experience some mild cramping and spotting, but these symptoms are usually temporary.
It’s essential to follow the doctor’s instructions carefully after the embryo transfer and to avoid activities that may harm the developing embryo, such as smoking or heavy lifting.
Step 5: Pregnancy Testing
Two weeks after the embryo transfer, the woman will undergo a pregnancy test to determine if the IVF treatment has been successful. This test measures the level of human chorionic gonadotropin (hCG) in the woman’s urine or blood.
If the test is positive, it indicates that the woman is pregnant. However, it’s essential to note that not all IVF treatments result in a successful pregnancy. The success rates of IVF vary depending on various factors, including the woman’s age, the number and quality of the embryos transferred, and the underlying cause of infertility.
If the pregnancy test is negative, it means that the IVF treatment was not successful. In this case, the woman may need to consider other treatment options or undergo another cycle of IVF.
If the pregnancy test is positive, the woman will need to undergo additional testing to monitor the pregnancy’s progress. This may include regular ultrasound scans and blood tests to check the levels of hormones in the body.
It’s important to follow the doctor’s instructions carefully during the early stages of pregnancy and to take any prescribed medications to ensure the best possible outcome.
Step 6: Pregnancy Monitoring and Delivery
After a successful IVF treatment, the woman will need to undergo regular monitoring throughout her pregnancy. This may include regular ultrasound scans and blood tests to check the developing baby’s growth and development.
The woman will also need to follow a healthy lifestyle during pregnancy, including a balanced diet and regular exercise, and avoid any activities that may harm the developing baby.
In some cases, the woman may need to take additional medications or undergo additional medical procedures during pregnancy to manage any underlying health conditions or complications.
As the pregnancy progresses, the woman will need to prepare for delivery and make plans for the birth of the baby. This may include choosing a hospital or birthing center and discussing the birth plan with the medical team.
The medical team will also discuss the various delivery options available, including natural delivery, induction of labor, or cesarean section, depending on the woman’s health and the baby’s condition.
During delivery, the medical team will monitor the mother and the baby closely to ensure safe and healthy delivery. After delivery, the woman and the baby will need to undergo regular monitoring to ensure their ongoing health and well-being.
Step 7: Postpartum Care
After delivery, the woman will need to undergo postpartum care to ensure a healthy recovery and to support the transition to parenthood. This may include regular check-ups with the medical team, as well as ongoing support from family and friends.
During postpartum care, the medical team will monitor the woman’s physical and emotional well-being and provide any necessary treatment or support. This may include medications to manage pain or any underlying health conditions, as well as counseling or support groups to address any emotional or psychological issues that may arise.
The medical team will also monitor the baby’s health and development during postpartum care, including regular check-ups and immunizations.
In addition to medical care, postpartum care may also involve practical support, such as assistance with breastfeeding, newborn care, and household tasks.
It’s essential for new parents to take care of themselves during postpartum care and to seek support as needed. This may include taking time off work or reducing other commitments to focus on the baby’s care and the transition to parenthood.
Step 8: Embryo Storage
Embryo storage is an important part of the IVF process for many couples, as it allows them to preserve any unused embryos for future use.
After the IVF treatment, any remaining healthy embryos can be frozen and stored for later use. Embryo storage allows couples to attempt another IVF cycle without the need for additional egg retrieval and can improve the chances of a successful pregnancy.
Embryo storage facilities typically use state-of-the-art technology to freeze embryos and maintain their viability over time. Embryos can be stored for many years, and the couple can choose to use them at any time in the future.
Embryo storage can also provide peace of mind for couples who may be facing a medical condition or treatment that could affect their fertility. By storing embryos, they can preserve their fertility and increase their chances of starting a family in the future.
It’s important to note that embryo storage can involve additional costs and may require ongoing payments for storage and maintenance. Couples should discuss the costs and options for embryo storage with their medical team and consider the long-term financial implications of this choice.
Step 9: Support and Follow-Up Care
After the IVF process is complete, it’s important for couples to receive ongoing support and follow-up care to ensure the best possible outcome for both the mother and the baby.
Support and follow-up care may involve regular check-ins with the medical team, as well as ongoing support from family and friends. This can help to monitor the mother’s physical and emotional well-being, as well as the baby’s development and any potential health issues.
It’s also important for couples to have access to resources and support groups that can help them navigate the challenges of parenthood, including sleep deprivation, stress, and postpartum depression. Many hospitals and healthcare facilities offer support groups for new parents, as well as resources for breastfeeding, newborn care, and other aspects of parenting.
In addition to medical care and support groups, couples may also benefit from counseling or therapy to address any emotional or psychological issues that may arise during the IVF process or after the baby is born. This can include anxiety, depression, or feelings of loss or grief related to infertility or other challenges.
Follow-up care may also involve regular check-ups and testing to monitor the baby’s health and development, as well as any ongoing medical needs or treatments.
Conclusion
The IVF process involves a series of steps, including ovarian stimulation, egg retrieval, fertilization, embryo culture, embryo transfer, and embryo storage. It’s important for couples to work closely with their medical team and understand each step of the process, as well as any potential risks or side effects.
Support and follow-up care are also essential components of the IVF process and can help to ensure the best possible outcome for both the mother and the baby. This can include ongoing medical care, support groups, counseling, and follow-up testing.
While IVF can be a costly procedure, many insurance plans now offer coverage for fertility treatments, including IVF. Couples should check with their insurance provider and medical team to determine their coverage options and any out-of-pocket costs.
In conclusion, the IVF process offers hope and the opportunity for parenthood to couples struggling with infertility. By working closely with their medical team, understanding each step of the process, and receiving ongoing support and follow-up care, couples can increase their chances of a successful pregnancy and a healthy and happy start for their new family.
FAQs:
- What is the success rate of IVF?
The success rate of IVF varies depending on a number of factors, including the age and health of the mother, the quality of the sperm and eggs, and the specific medical procedures used. On average, the success rate of IVF is around 40% for women under 35 and decreases with age.
- Is IVF a painful procedure?
The IVF process can involve some discomfort and pain, including bloating, cramping, and soreness following egg retrieval. However, the procedure is typically performed under anesthesia, and pain medication can be provided as needed.
- Are there any risks associated with IVF?
As with any medical procedure, there are some risks associated with IVF, including ovarian hyperstimulation syndrome, infection, and multiple pregnancies. However, these risks can be minimized with careful monitoring and appropriate medical care.